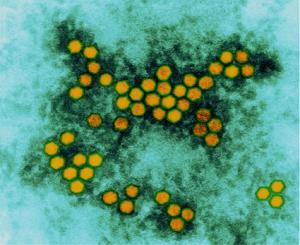
The oral vaccine for polio features the weakened form
of the poliovirus. Researchers are working to create a new
generation of vaccines that run no risk of reverting to
virulent states. Credit: Dennis Kunkel Microscopy, Inc.
SAN JOSE, Calif. — A million billion viral infections occur every second in the biosphere. And if the quadrillion quadrillion viruses inhabiting just the oceans were lined up, they would span the 120,000 light years of the Milky Way’s diameter a hundred times.
Most viruses don’t pose a danger to humanity, but some, such as HIV, influenza, enterovirus, and measles can be fatal. Protection against many viruses has come from the viruses themselves, through vaccines made from weakened or dead forms. But this method doesn’t work for more difficult targets, such as pathogens that change rapidly over time, cancers, or HIV. So researchers are looking to new technology for better solutions.
"The question is, can we make a synthetic virus-free vaccine? And, can we make it stable enough to be effective?" said Dave Stuart, who studies the structure of viruses at the Diamond Light Source synchrotron in Oxfordshire, U.K, during the American Association for the Advancement of Science annual meeting in San Jose, Calif.
Using the atomic structure and genetic code of viruses, researchers are reformulating the pathogens as vaccines by altering the genome or producing shells that lack genetic material.
Reverse vaccinology is a technique that involves sorting through the genome of the pathogen and seeking out features that identify the virus as “other” to the immune system. Those features can then be used to generate vaccines. That approach speeds analysis of candidate viruses.
“Now we can very rapidly go from thousands of genes on the genome to tens of genes, which is much more manageable,” said Jeffrey Ulmer, global head of external research at the pharmaceutical giant Novartis.
Synthetic vaccinology takes it a step further. Here, researchers begin with a benign virus and alter its shell so that it expresses the antigens — the red flags — that makes it look like a dangerous virus. This hybrid is not harmful, as it contains no disease-causing genetic material. Yet when it spreads throughout the patient, the body interprets it as a full-scale invasion and generates a long-lasting immune response. This method could speed vaccine creation.
“Conceivably, within a few weeks, you can go from declaration of an outbreak to having a vaccine,” Ulmer said.
Such a short timeline is crucial to inoculating the population as pandemics arise.
Another approach to designing vaccines is mutating large swaths of the virus genome. This takes advantage of the body’s naturally low frequency of certain pairings of some DNA sequences to help generate resistance to viruses. In the target virus, large sections of the genetic material are replaced with the rare DNA sequences.
“It turns out that actually the cells, seemingly, can recognize this virus much more easily than the wild type,” said Peter Simmonds of the University of Edinburgh. “Although the viruses are essentially nonpathogenic … and there is much less virus replication; what does occur is much more potent.”
There is no chance that these synthetic viruses will return to virulence, the researchers said.
“We’re putting in hundreds and hundreds of changes into the virus, and so none of these can collectively revert.” Ulmer said.
Marissa Shieh is a senior at Williams College majoring in chemistry. Reach her at marissa.shieh@gmail.com or follow her on Twitter @MarissaShieh.