By Adithi Ramakrishnan

SARS-CoV-2, the virus that causes COVID-19, gets its foot in the door by attaching to an external protein on human cells called ACE2, but new research suggests that another type of protein called an integrin could also be a promising target. Two complimentary studies show, for the first time, that integrins contain genetic sequences that direct the cellular housekeeping mechanism of autophagy, a process often exploited by viruses to enter cells and evade detection. Understanding how the coronavirus gets into the body is essential for developing ways to treat it, and a thorough understanding of the link between integrins, autophagy, and SARS-CoV-2 could help scientists repurpose existing medications to treat COVID-19.
“Viruses are complex, and they rarely target one receptor,” said Balint Mészáros, a postdoc at the European Molecular Biology Laboratory in Germany who coauthored one of two studies presented Feb. 8 at this year’s American Association for the Advancement of Science (AAAS) meeting. “Integrins have been known to be important [in maintaining healthy cells] for decades, and we now know that integrins directly regulate autophagy,” making them a potentially appealing target for SARS-CoV-2.
Scientists had discovered through work with viruses such as Zika and HIV that integrins, like ACE2, are valuable targets for slipping into human cells. While ACE2 regulates endocytosis, a process cells use to bring material—or in this case, viruses—in from the outside world, integrins were thought to be linked to autophagy, a process that helps cells clean out damaged cellular components.
Early in 2020, a group of Swiss researchers identified a sequence on the SARS-CoV-2 viral protein that integrins can bind to. Mészáros, who was researching integrins at the time, wondered if the novel coronavirus could hijack autophagy using such sequences.
To answer this question, Mészáros used bioinformatics to probe whether the genetic code of integrins contains any binding sites for proteins associated with autophagy—sites that could be juicy targets for SARS-CoV-2 to bind to instead. Once Mészáros identified several candidates, Johanna Kliche, a doctoral student at Uppsala University in Sweden who coauthored a second paper presented at AAAS, tested whether synthetic protein sequences from autophagy-related proteins actually did adhere to the suspected binding sites on integrins.
Together, the two identified a sequence within integrins’ genetic code that has a high binding affinity for proteins linked to autophagy, confirming that integrins have a role in directing the process and furthering scientists’ understanding of how SARS-CoV-2 might co-opt this mechanism.
Mészáros and Kliche also identified protein sequences on the ACE2 receptor that have a high affinity for proteins related to endocytosis. Because scientists have a better understanding of how SARS-CoV-2 enters cells using the endocytosis pathway, these findings helped confirm that bioinformatics and synthetic protein experiments are robust and useful tools for identifying potentially important binding sites, even in receptors other than ACE2.
“Based on this information, we can further complete this picture about how viral attachment works,” Mészáros said.
To make the final connection, however, future research will be necessary to confirm that the virus interacts with these specific sequences in cellular models.
This link between integrins and autophagy may make it possible for scientists to repurpose existing, FDA-approved drugs for treating COVID-19. In his paper, Mészáros compiled a list of candidate drugs, including the antipsychotic chlorpromazine—which inhibits endocytosis—and simvastatin, a drug that activates autophagy.
“Getting FDA approval for a compound can take a long time, and it’s a large investment from a company, but there are hundreds of thousands of compounds that we know are safe to administer to people,” Mészáros said. “There is a chance that some of these actually might work, we just don’t know.”
Mészáros and Kliche are hopeful that future studies will confirm the interactions between integrins, autophagy, and the coronavirus inside cells. Their work puts a spotlight on receptors other than ACE2 that could be vital agents in understanding and treating the novel coronavirus.
“The moral for us is that you have to keep looking,” Mészáros said. “In biology, if you keep poking at it, it’s more complex than you think—you’ll get new insight that might be useful.”
Adithi Ramakrishnan is a neuroscience major and creative writing minor at the College of William and Mary. She is a Summer Writing Award Winner from the National Association of Science Writers, a previous Pulitzer Center Student Fellow, and a contributor to Massive Science. Email her at aramakrishnan@email.wm.edu and follow her on Twitter @adithi718.
This story was edited by NASW member Amanda Heidt, who served as Ramakrishnan's mentor during the NASW-AAAS Spring Virtual Mentoring Program.
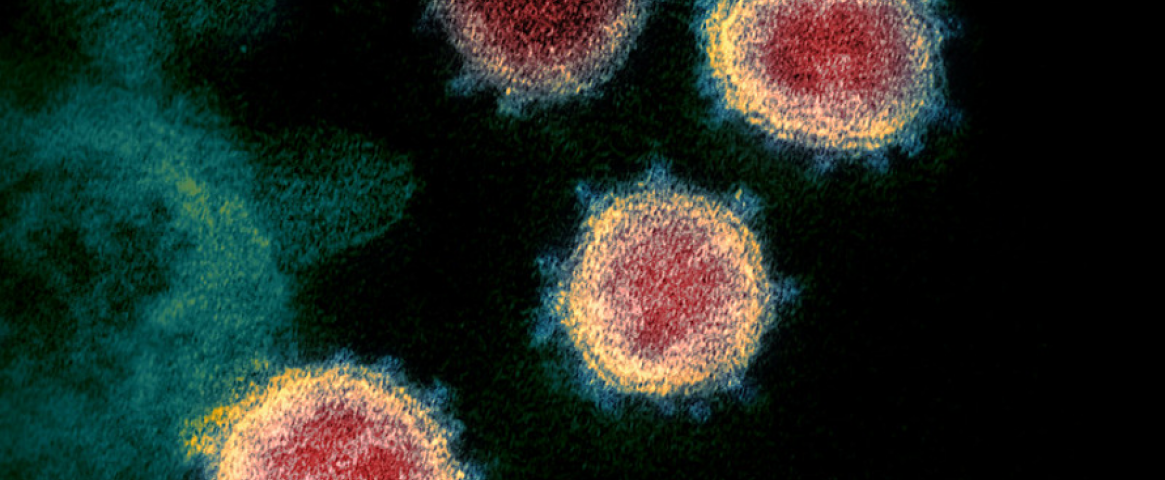
Hero image credit: NIAID.